What is Osteoarthritis?
Osteoarthritis (OA) is the most common form of arthritis. OA is associated with defective articular cartilage and can result in changes to the underlying bone. The damaged cartilage fails to act as a shock absorber and as a result the bones rub against each other, causing a lot of pain in that area. Factors like trauma, overuse of joints, joint instability and obesity can cause abnormal joint loading & increase the risk of OA. Aging also increases the likelihood of developing OA; as aging occurs, cartilage contains less water and fewer chondrocytes, thereby decreasing the capacity to restore and maintain the cartilage. In fact, more than 75% of people older than fifty-five show the joint deformations of OA on X-rays. But most of these people have no symptoms.
The damage to the cartilage seems to start a sort of chain reaction that involves all the parts of the joint. Bone spurs, or outgrowths, often begin to form around the edges of the joint. The joint capsule (the watertight sack around the joint) can become thickened and lose its stretch. The synovial membrane that lines the inside of the joint capsule may become inflamed (swollen, red, hot, and painful), and crystals may form in the synovial fluid. The tendons and ligaments around the joint can also become inflamed. Individuals with OA often develop bone formations around joint margins called osteophytes, or sclerosis (hardening) of subchondral bone.
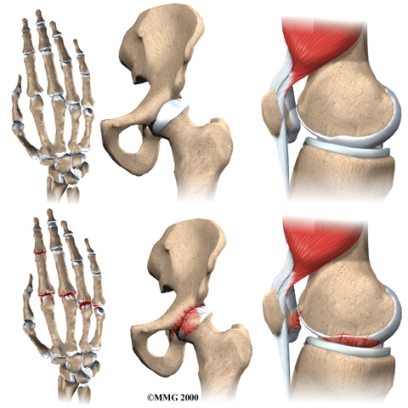
Heberden’s Nodes: hard or bony swellings that can develop in the distal interphalangeal joints (DIP) caused by formation of osteophytes (calcific spurs) of the joint cartilage secondary to trauma at the joint.
Bouchard’s Nodes: bony growths in the proximal interphalangeal (PIP) joints of the hand.
Where does OA develop?
OA is most common in the small joints of the hands, the spine, the knees, the hips, and certain toe joints. OA primarily affects the articular cartilage, the slippery, cushioned surface that covers the ends of the bones in most joints and lets the bones slide without rubbing.
Even the muscles around the joint can lose their strength. This usually occurs as a result of under-use of the muscles due to pain in the joint. When something hurts we subconsciously change the way we use the joint to avoid the pain. This causes the muscles to become weakened. Cartilage itself does not have nerves to feel pain, therefore the pain of OA probably comes from these other changes in and around the joint.
Symptoms
What does OA feel like? Patients with OA have one or more joints that are painful and stiff. The pain is a deep, dull ache that usually comes on gradually. Pain gets worse when the joint is used and gets better with rest. The joint is stiff after waking up or after not being used for some time, but the stiffness usually goes away fairly quickly. Over time the pain and the stiffness become almost constant.
No matter which joints are affected, OA patients report many of the same symptoms
-Most patients say that the pain is worse in cool, damp weather.
-Many OA patients feel or hear crackling or popping in the affected joints (called crepitus). This is most common in the knees.
-Joints enlarge or change shape. The enlarged areas are often tender to the touch.
-In most cases the affected joints can’t move through a normal range of motion.
-In other cases the joints have become so unstable that they can actually move too much or in the wrong direction.
Some symptoms depend on the affected joint. Patients with knee OA may have problems with the joint locking up, especially when they are stepping up or down. Patients with OA of the hip often limp. OA of the hands can affect the strength and movement of fingers and make simple tasks such as getting dressed very difficult. OA of the spine can cause neck and low back pain as well as weakness and numbness.
Our Treatment
There is no cure for OA, as it is a chronic but, in most cases a very manageable disease. Our goals of treatment at Health Bound Health Network are to relieve your pain and to improve or maintain the movement of your joints. Much of the treatment for OA involves no prescriptions at all. The physiotherapists at Health Bound Health Network will encourage you to take several steps to help manage your symptoms. Some interventions that we often recommend to our patients with OA are;
Exercise- there is some evidence suggesting that exercising can be a helpful intervention for patients with OA, however it may be counter-indicated in some instances, for example in case if the person’s joints are inflamed.
Do strengthening and range of motion exercises. These are most often taught and monitored by physical or occupational therapists.
Lose weight if necessary
Use heat and/or cold packs.
Tape the knee, if it is affected.
Prescribe custom made orthotics (insoles in your shoes) if the lower extremity is affected.
Receive massage.
Use adaptive equipment to help take pressure off your joints, such as a cane or special gadget to open jars.
Refer the patient to an Occupational Therapist who can create a custom hand splint (for example in case of thumb CMC OA)
Participate in education programs or support groups.
If you or a loved one have have been diagnosed with osteoarthritis contact us to speak with our team regarding your rehabilitation needs.


