
Pain Education
Pain arises for a multitude of reasons. Some pain lasts a short while such as when you touch something hot, whereas some pain can last for months or even years. The medical model categorizes pain as either acute or chronic (now known as persistent). Acute pain is short-term and is usually associated with bodily damage, once the injury has healed the pain subsides which lasts less than three months. According to Mills, Nicolson & Smith (2019), chronic pain is a leading cause of disability worldwide affecting approximately 1.9 billion people, the most common pain being recurring tension headaches. Chronic or persistent pain goes beyond 3 months and does not necessarily include bodily injury and is more attributed to the central nervous system.
How Does Pain Manifest?
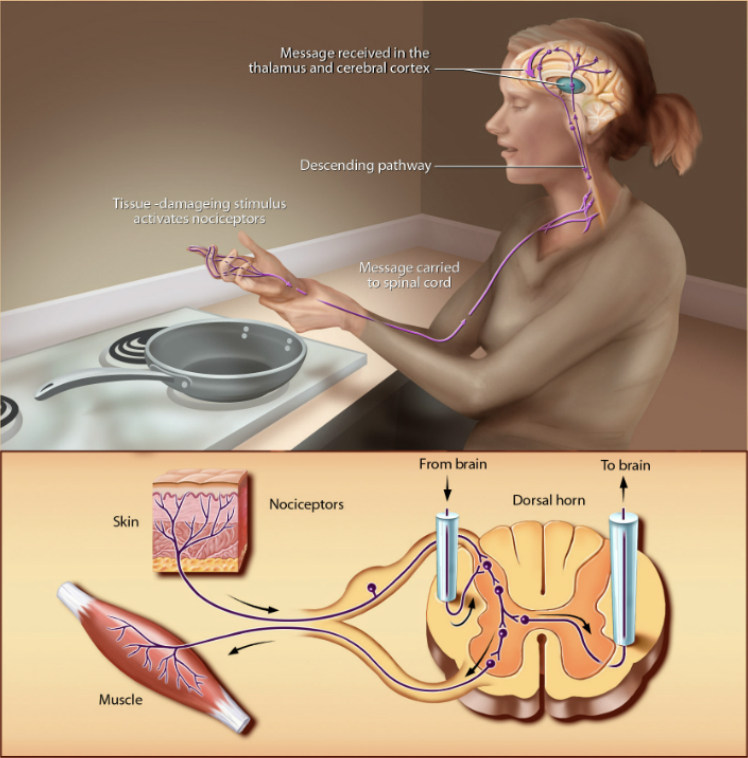
Although it may seem counterintuitive, pain is actually ingrained in the human systems to protect an individual from danger. For instance, when you were young you probably touched something hot such as a hot pan – this immediate signal was sent from nociceptors to the brain to identify a threat that tissues are at risk for damage. Nociceptors would fall under the umbrella of acute pain as the receptors are triggered by bodily injuries from either pressure or extreme temperatures (Dubin & Patapoutian., 2010). Chronic or persistent pain, however, can occur without the presence of tissue damage as it has emotional and cognitive factors that affect an individual’s perception of the pain (Crofford., 2015). The cognitive and emotional elements of chronic pain attribute to high levels of comorbid psychiatric disorders. For instance, 20-50% of people living with chronic pain have comorbid depression (Mills, Nicolson & Smith., 2019).
How Can You Manage Persistent Pain?
Research indicates that persistent pain management requires a multidisciplinary approach which may include the following: (Dydyk & Conermann., 2022)
- Physical Activity – increased activity can help an individual’s pain perception as the body releases natural pain relieving hormones known as endorphins. There are a wide range of activities that can accommodate an individual’s pain. For instance, if an individual suffers from chronic knee pain, activities that reduce weight bearing on the knees such as swimming would be beneficial.
- Pharmaceuticals – General practitioners may recommend non-opioid analgesics as a first line of treatment such as taking acetaminophen or NSAIDs (aspirin). This is due to the high risk of dependency an individual can develop when taking Opioid analgesics.
- Non-pharmaceuticals therapies – apply hot and cold compresses, cognitive behavioural therapy, and counselling.
References
Crofford L. J. (2015). Chronic Pain: Where the Body Meets the Brain. Transactions of the American Clinical and Climatological Association, 126, 167–183.
Dubin, A. E., & Patapoutian, A. (2010). Nociceptors: the sensors of the pain pathway. The Journal of clinical investigation, 120(11), 3760–3772. https://doi.org/10.1172/JCI42843
Dydyk AM, Conermann T. Chronic Pain. [Updated 2022 May 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553030/
Mills, S., Nicolson, K. P., & Smith, B. H. (2019). Chronic pain: a review of its epidemiology and associated factors in population-based studies. British journal of anaesthesia, 123(2), e273–e283. https://doi.org/10.1016/j.bja.2019.03.023
Understanding Persistent Pain. Department of Health and Human Services. 2022. https://www.brainfacts.org/thinking-sensing-and-behaving/touch/2012/touch-and-pain

