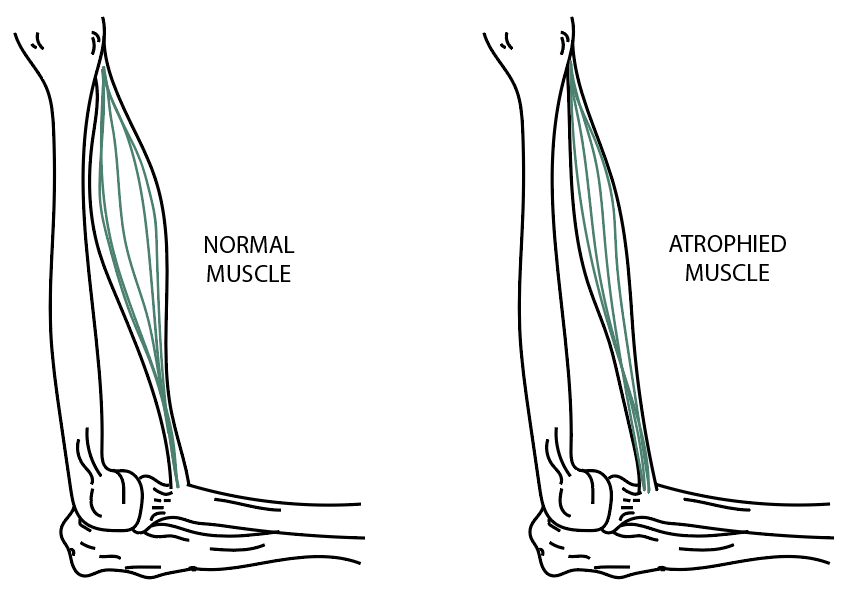
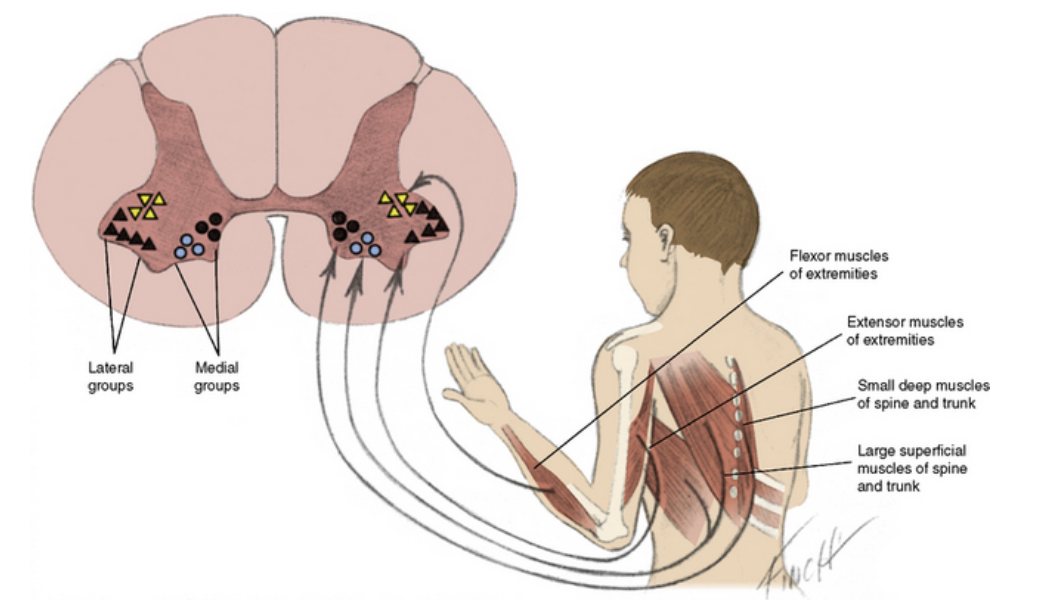
Spinal Muscular Atrophy (SMA) is a recessive genetic disease that causes progressive degeneration of the anterior horn cells in the spinal column (Burr & Reddivari., 2021). The degeneration of the anterior horn cells results in muscle weakness, muscle atrophy, and breaks down motor neurons along the spinal cord (Burr & Reddivari., 2021). The incidence of SMA is approximately 1 in 10 000 births and the carrier frequency is 1:50 (Shababi et al., 2014). Clinically there are 4 types of SMA that have been identified which are categorized based on an individual’s motor function and age of onset (Kolb & Kissel., 2015). However, there has been the addition of type 0 for newborns who usually die within the first month of life due to respiratory failure (Kolb & Kissel., 2015). Individuals are categorized into the types of SMA (1-4) based on developmental milestones, symptom onset, and life span (Shababi et al., 2014).

Clinical Manifestations (Burr & Reddivari., 2021)
SMA Type 1 aka Werdnig-Hoffman Disease
- Also known as non-sitters
- Lifespan is usually less than 1 year of life
- Demonstrate to have limited control of the head, decreased muscle tone, and absence of tendon reflexes and continues to progressively decline
- Weakness of the intercostal muscles that assist with respiratory function, leads to a bell-shaped chest
- Swallowing difficulties which are correlated with failure to thrive and the risk of aspiration
- Cognition is normal
SMA Type 2 aka Dubowitz Disease
- Able to sit without support
- Not being able to walk independently
- Muscle leg weakness
- Bone and joint development is abnormal which can result in progressive scoliosis, joint contractures, and ankylosis
- Restrictive lung disease
- Cognition is normal
SMA Type 3 aka Kugelberg-Welander Disease
- Can walk without supports at some point during their lifetime, however, as muscle weakness begins to affect the legs this will lead to the individual requiring a wheelchair
- Those with SMA Type 3 are less likely to develop scoliosis and restrictive lung disease
- Life expectancy and cognition are not affected
SMA Type 4 – Adult Onset
- Mildest form of the disease and represent less than 5% of SMA cases
- Similar to type 3
- Onset develops after 30 years of age
SMA Management
In 2004, to improve the quality of life for those living with SMA a committee of experts provided a statement on standard of care (Mercuri et al., 2018). The committee produced a set of guidelines concentrating on a multidisciplinary team approach that focuses on rehabilitation, orthopedic, pulmonary, nutritional, and palliative care (Mercuri et al., 2018). Some team members include; neurologists, geneticists, pediatric surgeons, orthopedic surgeons, physiotherapists, occupational therapists, and nutritionists (Burr & Reddivari., 2021).
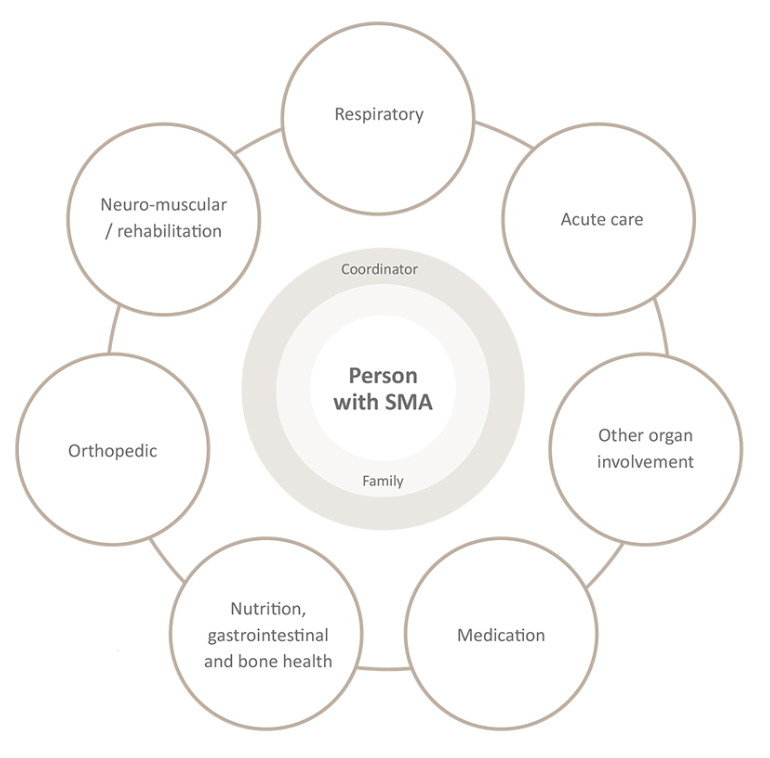
Physiotherapy and Occupational Therapy
Physiotherapy and Occupational therapy are forms of rehabilitation that can be incorporated into a treatment plan for an individual with SMA. Physiotherapy will focus on providing care to maintain functional ability, people living with SMA present with joint contractures which makes moving joints difficult and painful (International Standards of Care., 2017). Occupational therapy can provide adaptive equipment and mobility exercises to make activities of daily living more manageable (International Standards of Care., 2017).
References
A guide to the 2017 – treat-NMD. (n.d.). Retrieved July 4, 2022, from https://treat-nmd.org/wp-content/uploads/2019/06/uncategorized-A-Guide-to-the-2017-International-Standards-of-Care-for-SMA_UKEnglish_Digital-v2L.pdf
Burr P, Reddivari AKR. Spinal Muscle Atrophy. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560687/
Kolb SJ, Kissel JT. Spinal Muscular Atrophy. Neurol Clin. 2015 Nov;33(4):831-46. doi: 10.1016/j.ncl.2015.07.004. PMID: 26515624; PMCID: PMC4628728.
Mercuri E, Finkel RS, Muntoni F, Wirth B, Montes J, Main M, Mazzone ES, Vitale M, Snyder B, Quijano-Roy S, Bertini E, Davis RH, Meyer OH, Simonds AK, Schroth MK, Graham RJ, Kirschner J, Iannaccone ST, Crawford TO, Woods S, Qian Y, Sejersen T; SMA Care Group. Diagnosis and management of spinal muscular atrophy: Part 1: Recommendations for diagnosis, rehabilitation, orthopedic and nutritional care. Neuromuscul Disord. 2018 Feb;28(2):103-115. doi: 10.1016/j.nmd.2017.11.005. Epub 2017 Nov 23. PMID: 29290580.
Shababi M, Lorson CL, Rudnik-Schöneborn SS. Spinal muscular atrophy: a motor neuron disorder or a multi-organ disease? J Anat. 2014 Jan;224(1):15-28. doi: 10.1111/joa.12083. Epub 2013 Jul 22. PMID: 23876144; PMCID: PMC3867883.

